Arab Health Issue 2 2012
Nice article outlining how to decide what to do when someone sustains ACL Injury.
Why Did Kobe Go to Germany?
An aging star and the new procedure that could revolutionize sports medicine
By Jonah Lehrer onThis is not the usual curve of an NBA career. As the economist David Berri has demonstrated, most NBA players exhibit an inverted U curve of productivity, showing a steep ascent as they first learn to play in the NBA. Their peak arrives shortly thereafter, usually around age 24 or 25, and is followed by a steady plateau until age 27. It's at this point that the decline begins: The grind of the season starts to dismantle the body. Joints give out, muscles lose their fast twitch fibers, tendons are torn. It's the usual tragedy of time, only accelerated by the intensity of professional basketball. By the age of 30, their glory days are probably long gone.
And yet, the aging Kobe — he will turn 34 this summer1 — seems to have resisted this dismal downward arc. In particular, Kobe's arthritic right knee seems to have healed itself, allowing him to return to more aggressive form. As Mike Brown, the Lakers coach, noted in December: "He's done some things in practice that have kind of wowed you as far as taking the ball to the basket strong and finishing with dunks in traffic." Kobe concurs: "I feel a lot stronger and a lot quicker."
Although Kobe has been mostly silent on the topic of his arthritic knee — "I'm not talking about my injury" is a constant refrain — his main treatment consisted of a new therapy called Regenokine. The therapy itself is part of a larger category of treatments known as "biologic medicine," in which the patient's own tissues are extracted, carefully manipulated, and then reintroduced to the body.
In recent years, there has been an explosion of interest in biologics. (The list of people who have also experimented with Regenokine reportedly includes Fred Couples, superagent Ari Emanuel, and the late Pope John Paul II.) Those willing to pay out of pocket can now treat their ailing joints with everything from platelet rich plasma (PRP) therapy, in which blood is spun until it contains a high concentration of healing platelets, to concentrated bone marrow injections, dense with stem cells. What all of these biologics have in common is the same appealing logic: Instead of cutting with a scalpel, or administering a synthetic drug — these treatments have long recovery times and nasty side effects — the healing mechanisms of the flesh should be put to work. The body heals best when it heals itself.
Kobe is clearly a believer in Regenokine and biologic medicine. Last July, he traveled to Düsseldorf, Germany, for an experimental version of the treatment and, according to reports, returned for a second round in October. He even recommended the treatment to Alex Rodriguez, which led the baseball star to undergo the same treatment on his knee late last year. Bryant hasn't commented publicly on the treatment, but A-Rod has described the feelings of his friend. Bryant "was really adamant about how great the procedure was for him," Rodriguez told reporters."I know that he was hurting before, almost even thinking about retirement, that's how much pain he was under. And then he said after he went to Germany he felt like a 27-year-old again. I was still a little apprehensive about it and he kept staying on me about it."
The reason Kobe, A-Rod, and other athletes travel to Germany for their biologic treatments involves a vague FDA regulation that mandates that all human tissues (such as blood and bone marrow) can only be "minimally manipulated," or else they are classified as a drug and subject to much stricter governmental regulations. The problem, of course, is figuring out what "minimal" means in the context of biologics. Can the blood be heated to a higher temperature, as with Regenokine? Spun in a centrifuge? Can certain proteins be filtered out?2 Nobody knows the answer to these questions, and most American doctors are unwilling to risk the ire of regulators.
The lack of clear FDA approval also reflects the larger uncertainty over biologic medicine. After all, many of these procedures are only a few years old, which means there is scant proof of their effectiveness. As a result, the case reports of athletes represent an interesting test of the medicine. Their performance on the field is a kind of clinical trial.
If Kobe and these proponents of biologic medicine are right, it will represent a stunning advance in sports medicine. While most athletes have been forced to undergo surgery after suffering joint damage — Kobe has undergone several procedures himself, with mixed results — biologic therapy holds out the enthralling possibility that these injuries can be reversed. Furthermore, such therapies are typically done on an outpatient basis, with recovery times measured in days, not months.
The alternative, of course, is that Regenokine, PRP therapy and stem cell injections are merely the latest overhyped medical treatments for desperate athletes, risky procedures that have yet to be properly vetted by rigorous clinical trials. Given the paucity of evidence, it's entirely possible that these biologic treatments will one day be consigned to the trash bin of experimental medicine, a set of therapies that are little more than an expensive placebo. Perhaps Kobe's knee isn't really healed — he just thinks it is.
The Orthohealing Center is located on a dreary stretch of Santa Monica Boulevard in West Los Angeles, stuck in one of those neighborhoods where the closest landmark is a freeway. Dr. Steven Sampson, a founder of the Center, is a clinical instructor at the David Geffen School of Medicine at UCLA. He has a boyish, unlined face — the only sign of age is a spreading bald spot — and a frantic, impatient energy. Even while talking to patients, he flits about the room, rushing between the injured joint and the ultrasound machine. The only time I saw him sit still was when he gulped down his salad while taking me through his favorite powerpoint presentation.
"The patients we treat need to move," Sampson says. "These people can't sit still. Sometimes, that's because their career depends upon their body. But most of the time it's just because they derive great satisfaction from exercise and sports." Sampson estimates that between 5 and 10 percent of his patients are professional athletes, competing in sports ranging from track and field to soccer, from the NBA to the NFL.
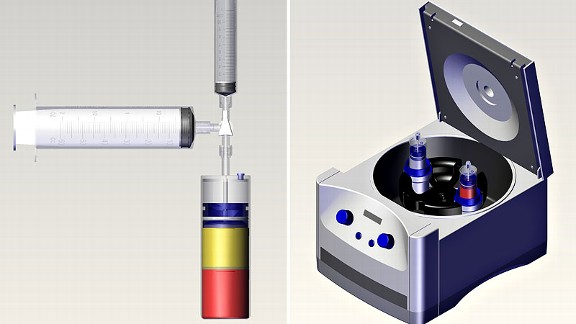
Sampson is a pioneer of PRP therapy, the most popular and accessible biologic treatment. (Injections start at $500.) Unlike Regenokine, PRP therapy does not involve the incubation of blood or any attempt to select for particular anti-inflammatory proteins. Instead, the patient's blood is merely spun in a centrifuge at high speed, until a layer of liquid rich in platelets appears in the plastic vial. (The goal is to achieve a platelet concentration that's at least three times higher than normal.) Because platelets are associated with the healing process — they keep us from bleeding out, but they also trigger tissue regeneration — the hope is that the platelet-rich liquid will accelerate recovery.
Sampson first discovered PRP therapy while working as a resident for an orthopedic surgeon who treated several European soccer players. "They were the first ones to tell me about blood spinning," Sampson remembers. "They'd talk about this amazing new procedure, how they were recovering from joint injuries in half the time. I thought it sounded way too good to be true."
However, when Sampson looked into the logic behind the treatment, he became intrigued. "What's more natural than your own blood?" Sampson asks. "All we're doing is amplifying the body's own healing mechanism. And we're doing this in the most minimal way possible. There's no adverse reaction, no immune response, because it's your blood. Only better."
Of course, many treatments that sound promising fail to pass the rigorous testing phase, in which they must outperform placebos in controlled trials. And the results from PRP therapy are complicated. Some clinical studies, such as a 2010 double-blind trial in the Netherlands that compared PRP treatment to injections of saline solution, found no significant difference in pain level two years after the injury. The authors concluded that the benefits of PRP therapy are most likely due to physical therapy, and not the injections of blood.
And yet, there's also evidence of PRP's success, even if the results remain modest. One of the most widely cited trials involved patients suffering from tennis elbow, a tendon injury caused by overexertion.3 The trial, led by Allan Mishra at Stanford University, looked at 15 patients suffering from serious tennis elbow. They were given a standard PRP injection, while a control group was given an injection of local anaesthetic. While the majority of those in the control group sought alternative treatments — and were thus excluded from the study — more than 93 percent of those in the PRP group were "extremely satisfied" with the treatment after one year.
Sampson has led a pilot study looking at the use of PRP therapy for knee osteoarthritis, which is what Kobe and many other young athletes suffer from. "These athletes are so tough on their bodies that we see people in their mid-twenties coming in with bone-on-bone joints," he says. "If they were older you might suggest joint replacements. But that's not feasible in someone so young."
Sampson's initial results suggest that PRP therapy can alleviate many arthritic symptoms, with the average patient reporting a significant decrease in knee pain after 16 weeks of treatment. (He also observed a thickening of cartilage in the joint, suggesting that real healing was taking place.) Follow-up studies confirm these optimistic results, at least in younger patients.
Perhaps the most convincing proof, however, comes from a controlled study of 120 patients given either PRP injections or hyaluronic acid, a lubricant that is often used to provide relief for arthritic joints. According to the data, those given PRP injections reported significantly better outcomes than those given the lubricant, with an average 60 percent decrease in painful symptoms.
Nevertheless, even ardent proponents of PRP therapy admit that it's still too soon to know for sure if the treatment is actually effective. (As one surgeon told me, "As soon as I walk into the room with a patient, they're going to experience a big reduction in pain. A lot of people in these trials want to get better, and that makes all the difference.") Sampson himself notes that inconsistencies in the application of PRP therapy — some doctors use lower platelet concentrations, or inject the blood in the wrong place — make it difficult to properly assess the treatment. As a result, modern medicine remains dependent on human guinea pigs like Kobe and A-Rod, these professional athletes willing to spend tens of thousands of dollars on unproven medicine.
When I ask Sampson about the outcomes he sees among his own patients, he tries hard to contain his enthusiasm. "You have to remember that I'm treating people who have tried everything else," he says. "They've done the cortisone injections. They've done acupuncture and physical therapy. Maybe they've even gone under the knife. And they come here because they don't know what else to do."
And yet, according to Sampson, approximately 65 percent of these chronic sufferers get better. I then ask him for his favorite success story. His face erupts in an embarrassed smile. "There was this soccer superstar — I can't tell you his name — who came to me two days before the championship game," he says. "And he had suffered an ugly joint injury. I was a bit nervous, because there really was no margin for error given the time frame. But I applied PRP therapy and he was able to compete. I remember one of the commentators on the TV wondering how he healed so fast."
What makes these anecdotes more alluring, at least for those whose livelihood depends upon their bodies, is that orthopedic medicine remains a fraught practice. Consider an influential 2002 trial that compared arthroscopic surgery for knee osteoathritis to a sham surgery, in which people were randomly assigned to have their knee cut open but without any additional treatment. (The surgeon who performed all the operations was the orthopedic specialist for an NBA team.) The data was clear: there was no measurable difference between those who received the real surgery and those who received the fake one. If anything, those in the treatment group actually appeared worse off than those in the placebo group. Nevertheless, surgeons continue to perform hundreds of thousands of arthroscopic procedures to treat this chronic knee condition.
These disappointing results help explain why so many elite athletes are willing to conduct medical experiments on themselves. It's why Peyton Manning and Bartolo Colon had stem cells injected into their ailing bodies and why Sampson is currently seeding bone marrow taken from the hip into the wrecked ankle of a pole vaulter. ("She's desperate to compete in the Olympic trials this summer," he says. "And nothing else has worked.") It's why soccer stars were the first subjects for PRP therapy and why Kobe's comeback has triggered a surge of interest among professional athletes for blood spinning and biologics. In many instances, these athletes are seeking treatment without telling their trainers, who remain wedded to older techniques. "For a lot of doctors, blood spinning still seems like this crazy and unproven approach," Sampson says. "They don't believe the evidence so far, which is why they insist on surgery and cortisone injections, even though both those treatments can make things worse.4 But it won't be that way for long. Injecting yourself with your blood won't always seem so strange."
In fact, Sampson argues that Jeremy Lin should have tried PRP therapy for his meniscus tear instead of opting for surgery. While noting that he doesn't have access to all the facts, Sampson describes similar patients who have had the torn flap of cartilage removed. "These athletes can demonstrate full cartilage loss in just three to four months after the operation when returning to sport," he notes. Sampson describes such surgeries as a "band-aid treatment," easing the immediate pain but at the risk of extensive long-term damage. "You've got to consider the entire career," he says.
And that's why Sampson advocates PRP therapy for people in Lin's situation. "A chronic tear has poor blood flow and slowed healing capacity," Sampson wrote in an email. "The PRP injection may stimulate the natural repair of the body with little downtime, at least compared to the surgical option." Of course, such an approach might also have allowed Lin to keep on playing. The treatment would not have ended his season.
Chris Renna is one of the only doctors administering Regenokine in the United States. He currently operates two clinics, located in Dallas and Santa Monica. While Renna is "slightly concerned" about possible FDA action, he's confident that they will uphold his right to treat the aches and pains of his patients with their own blood, especially given all the interest in Regenokine post-Kobe. "I'm convinced that this treatment should be the standard of care for the treatment of osteoarthritis and lower back pain," he says. "It shouldn't be reserved for professional athletes or movie stars or those people who can pay out of pocket. Regenokine isn't a panacea, but it's still far better than anything else we've got."
As with PRP therapy, there is some initial evidence to support such claims. The best demonstration of Regenokine's effectiveness comes from a 2008 study in which 376 patients were either given injections of saline, hyaluronic acid or manipulated blood. Although only 32 percent of the saline and hyaluronic acid patients saw a dramatic reduction in pain, more than 67 percent of Wehling's patients reported feeling much better. According to Renna, when Regenokine is combined with lifestyle changes, such as improved diet and sleeping routines, his success rate nears 90 percent. "I'm the first one to say that we need more evidence," he says. "But I also think the evidence so far strongly suggests that the improvements I'm seeing in my patients is real, especially when you compare Regenokine to the data from more conventional treatments. "
Pain, of course, is a slippery phenomenon, a condition that begins in the body but unfolds in the mind. And this is why it's impossible, at least so far, to separate the healing benefits of biologic medicine from our belief in its benefits.
Because this is a treatment we want to believe in. For the first time, professional athletes have been given access to a legal therapy that promises to reverse their inevitable decline, restoring those joints that have been worn away by a lifetime of competition. The inverted U curve of performance haunts the career of every veteran; the nightmare of the gifted is the loss of their gift. If biologic medicine does nothing else, at least it assuages this anxiety, giving aging stars a newfound sense of confidence. As Kobe's season appears to demonstrate, the curve can be reversed.
Of course, it's still far too soon to know if Kobe has found a cure for his broken down knee. (He has yet to find a cure for his ball hogging or for his current shin injury, which can't be treated using biologic medicine.) Perhaps the reduction in pain and inflammation is real. Perhaps we are on the cusp of a revolution in sports medicine, in which superstars find a way to extend their careers. Or maybe the injection of spun blood is just an elaborate placebo, a high-tech gimmick that tricks the brain into disbelieving the laments of the body.
But sports stars can't wait for the truth to accumulate; clinical trials take way too long. Their clock is ticking.



